Every year, tens of thousands of surgical patients are affected by anesthesia errors. While relatively rare, these mistakes – often caused by medical malpractice – can have severe consequences. Patients who receive too little general anesthetic can awaken suddenly during surgery, experiencing extreme pain and panic. Administering too much anesthesia can be just as damaging, even fatal.
While most patients focus their attention on the surgeon performing an operation, anesthesiologists are critical players in patient care. Complex modern surgeries are only possible because of safe and effective anesthesia. Before anesthetics drugs were developed, surgeons had little more to dull the pain of an operation than alcohol and opium.
Anesthesiologists are doctors. Like every other physician in America, anesthesiologists complete four years of medical school, and then go on to finish a residency in anesthesia, which generally lasts three years. Many anesthesiologists have also completed fellowships in specific fields of anesthetic practice, according to New York’s Hospital for Special Surgery, like regional anesthesia or pediatric anesthesia.
These are specialists, highly-trained professionals who must be held to a rigorous standard of care. Anesthesia is dangerous, and even slight mistakes in dosage or administration can lead to tragic results:
When healthcare professionals deviate from existing standards of care, violating well-established guidelines in the medical community, they can be held accountable in a medical malpractice lawsuit. Our New York City medical malpractice lawyers help guide victims through the process of filing these lawsuits.
Anesthesia is how trained medical professionals manage the amount of pain patients experience during surgical procedures. The purpose of anesthesia, and thus of an anesthesiologist, is to ensure that patients don’t feel the pain and discomfort that surgical operations would otherwise cause.
To do so, anesthesiologists rely on drugs that interrupt or depress nerve function. Nerves are fibers that communicate electrical signals between muscles, organs and the central nervous system, the brain and spinal cord. In a basic sense, nerves are the reason we feel anything, including pain.
Anesthesiologists use three basic types of anesthesia to knock out these pain signals:
While not technically an anesthetic, sedation drugs are often used in conjunction with anesthesia, to relax patients and create a sense of drowsiness. Unlike general anesthesia, sedatives do not – or should not – induce unconsciousness.
Choosing the appropriate type of anesthetic, the correct drug, is the first step in managing pain properly. Although some anesthesiologists will consult with patients beforehand and consider individual preferences, most doctors rely on past medical history, along with the results of medical tests, to decide on the appropriate anesthetic.
Determining how much anesthesia to administer is just as important, and body weight is only one factor that anesthesiologists should consider. Age and preexisting health conditions must also be taken into account. Even a patient’s ethnicity can be a key component of calculating the proper dosage, according to Pei-Shan Zhao MD, an anesthesiologist and associate clinical professor at Tufts University Medical School. Asian patients, for example, are more sensitive to opioid-based anesthetics than Caucasian patients, Zhao says.
Administering anesthetic drugs is a complex technical procedure. Spinal anesthetics present a particular risk, as the anesthesiologist’s needle pierces dangerously close to a patient’s spinal cord. Once a drug has been given, continuous monitoring of a patient’s vital signs is critical. Blood pressure, heart rate and blood oxygen levels must be maintained at safe levels to prevent harm.
After going under general anesthesia, patients require medical assistance to breath. In most cases, a breathing mask or endotracheal tube, inserted through the mouth, will be used to supply the patient’s body with oxygen.
Intubation errors, however, are common. Inserting a breathing tube can be difficult and repeated attempts at intubation can lead to tracheal damage. In rare cases, negligent monitoring can lead to asphyxia, or oxygen deprivation, increasing the risk of organ damage and brain injuries.
Anesthesiologists use an array of technologies to monitor the depth of anesthesia, ensuring that patients don’t gain awareness during surgery. Despite these prevention measures, patients gain consciousness during procedures at alarming rates.
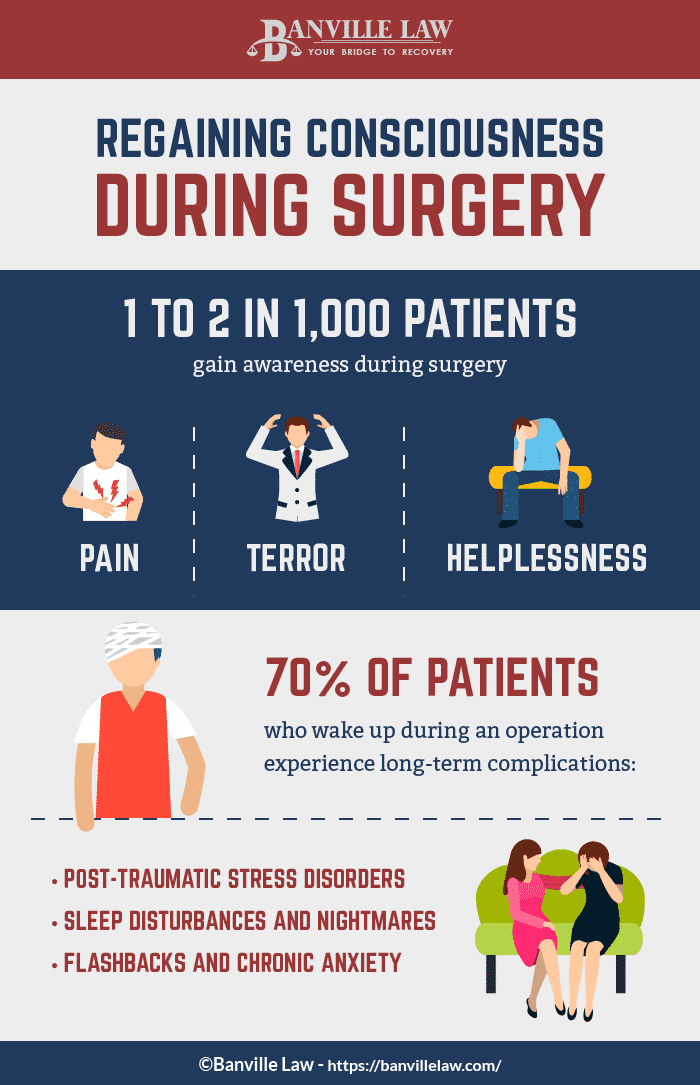
Between 1 and 2 out of 1,000 patients become aware during surgical operations, researchers at Emory University say, amounting to 26,000 patients per year.
Regaining consciousness can be terrifying, even in the absence of pain sensations. Patients frequently experiencing extreme terror, anxiety and distressing feelings of helplessness. Post-traumatic stress disorders are not uncommon. In one study, researchers in Amsterdam found that up to 70% of patients who wake up during surgery will experience long-term complications, from sleep disturbances and nightmares to flashbacks.
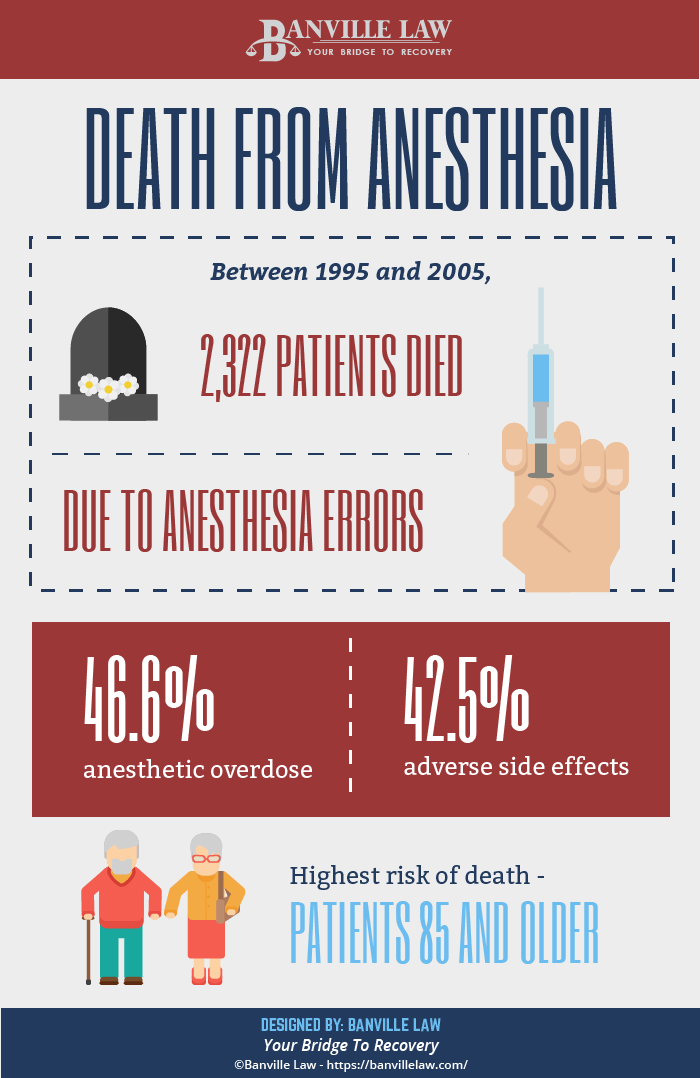
Anesthesia can be fatal. In fact, at least 387 people died every year between 1999 and 2005 due solely to anesthesia errors. Nearly 50% of those patients were killed by anesthetic over-administration. The remaining half died after experiencing adverse side effects, including allergic reactions.
Anesthesia-related deaths are nearly always preventable – a clear example of medical negligence. Surviving family members may be eligible to file a wrongful death lawsuit, seeking compensation for funeral expenses and healthcare expenses, along with pain and suffering.
Continue reading: Failure To Diagnose & Misdiagnosis Lawsuits