Hysterectomy, the surgical removal of the uterus, is an operation that women commonly undergo in order to alleviate uterine conditions that are significantly detrimental to their health and well-being.
However, a certain device often used in minimally-invasive hysterectomies, the power morcellator, has been found to spread undiagnosed uterine cancer, severely threatening a patient’s health and chance of cancer survival.
The discovery of such dire consequences prompted the FDA to issue a set of serious warnings in April 2014, leading to an aftermath of ongoing developments and debate among patients, medical professionals, device manufacturers, the media, and government officials.
Some background on the uterus itself can be helpful in understanding possible issues surrounding hysterectomies.
The uterus, commonly referred to as the womb, is an organ in the female reproductive system that serves many important functions.
The uterus aids sperm transport during sexual intercourse, houses and nourishes fertilized egg(s) during pregnancy to allow growth and development through the embryonic and fetal stages, facilitates childbirth via contractions, and lends structural support for the bladder and the bowels.
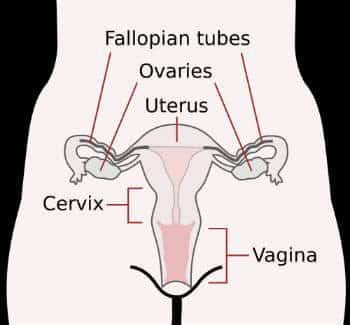
Anatomically, the uterus is located centrally within the pelvis and is comprised of two main parts—the uterus body (corpus uteri), which is the triangular top portion, and the cervix, the narrower bottom portion that is connected to the vagina. The ovaries lie on either side of the uterus and are connected to it via the Fallopian tubes.
See more on morcellator's here: https://banvillelaw.com/morcellator/
In addition to the uterus playing such a central role in the female reproductive system, as well as providing structural support within the pelvis, many women also harbor an emotional attachment to it as an element in their sense of female identity.
This is why hysterectomy is usually an option only pursued for conditions that seriously affect a patient’s health and/or quality of life, and only after all alternative treatments have been explored without success.
Such conditions can include:
However, the most common reason for having a hysterectomy is to end discomfort, pain, abnormal bleeding, bowel/bladder obstruction, and other adverse symptoms resulting from the presence of uterine fibroids, benign growths in the uterine muscle wall.
Dr. Jennifer Brown at Everyday Health has written a comprehensive discussion of hysterectomy facts and myths.
The various types of hysterectomies available are differentiated based on which exact part(s) of the uterus and/or associated organs are removed:
Patients may opt for a partial hysterectomy if cervical cancer is not a concern. Possible benefits include greater retention of pelvic structure and sexual function after surgery.
The ovaries secrete and regulate hormones that are crucial to reproductive functioning and overall health in the childbearing years, but that can also contribute to the development of breast cancer.
Therefore, patients may be urged to have this type of hysterectomy if ovarian or breast cancer is a concern, especially if the patient no longer plans to have children. However, patients must also consider the fact that ovary removal causes menopause to occur.
Though open surgery is still the most common option for hysterectomies, according to the UNC School of Medicine, recent decades have seen a rise in popularity of less invasive methods that appeal to patients by promising a speedier or less difficult recovery period. More information on the following methods can be found here.
In this procedure, access to the uterus is provided by making a 5 to 7 inch incision, either vertically or horizontally, in the abdomen, which leaves a scar after recovery. Manual surgical tools and traditional techniques are used to carry out the operation.
Patients typically stay in the hospital for several days post-operation, and complete recovery commonly requires 6 to 8 weeks.
This procedure, performed through a vaginal incision, involves detaching the uterus from the fallopian tubes, upper vagina, and any other connected tissue, and removing it via the vagina.
Time required for complete recovery is typically 3 to 4 weeks, and the surgery leaves no visible scar. However, this option is not viable for an enlarged uterus.
This method uses a laparoscope (a long, thin tube used for vision and illumination of internal organs) inserted through small (1/4 to ½ inch) incisions in the abdomen to aid in removing the uterus vaginally.
It has a short recovery time of about 2 weeks and only leaves small abdominal scars, but just as in vaginal hysterectomy, is not viable for an enlarged uterus, and also cannot be performed on women who have undergone cesarean section.
One of the least invasive methods currently available, the laparoscopic hysterectomy is performed via laparoscopic tools and involves cutting up the uterus into tiny pieces for removal through the small abdominal entry incisions.
This method has grown in popularity since its development in the early 90’s, likely because of its reputation for minimal post-operative scarring and pain, and for very short recovery periods (sometimes lasting less than 2 weeks).
However, one of the instruments used to cut/shred up the uterus in this procedure, the power morcellator, operates via spinning blades that can easily disperse tissue fragments. If the patient has undetected uterine cancer, such dispersal can spread the cancer and escalate it to a serious stage, leading to possible grave effects on the patient’s health and life expectancy.
Especially alarming is the fact that there is no reliable non-surgical method of testing for leiomyosarcoma, one of the most lethal forms of uterine cancer.
Though leiomyosarcoma is relatively rare, comprising only about 3% of all uterine cancers, it is associated with very poor survival rates even with early detection.
Leiomyosarcoma is notoriously difficult to detect prior to surgery because the cancer’s tumors closely resemble uterine fibroids (which are benign) in appearance. Furthermore, a majority of prospective hysterectomy patients possess risk factors for uterine cancer.
Many significant events have occurred in response to the 2014 FDA warnings against the use of power morcellators, including a worldwide recall of power morcellator models by a leading manufacturer, banning of the devices in certain hospitals, retraction of coverage for procedures involving morcellation by insurance companies, and even legislative changes regarding the monitoring of medical devices.
A number of lawsuits have surfaced that allege that morcellator manufacturers and/or medical professionals have either been negligent or misleading in informing patients of the possible risks of and/or available alternatives to morcellation.
As we’ve seen earlier in this article, there are sound alternatives to laparoscopic hysterectomies that should be mentioned to prospective patients.
If you or a loved one may have been harmed after undergoing a procedure employing power morcellators, it would be wise to explore your legal options for obtaining justice and possible compensation for your hardship. The personal injury attorneys at Banville Law have experience representing victims and getting them the compensation they deserve. The firm is located in Manhattan and has represented clients in all boroughs and counties of the city as well as throughout the state. Contact Banville Law for a free consultation today.